Suppose two people see a doctor and complain about joint pain. One was diagnosed with arthritis and the other was diagnosed with arthritis. When two patients sit together, they have time to discuss their health issues.
It turns out that their symptoms are very similar: joint injuries, they did not bend/straighten with maximum strength, and did not rest at night or during the day. Even the diagnosis is consonants, but there are still differences. If both diseases affect the joints, what is the difference between arthritis and arthritis?
What is arthritis
Arthritis is an inflammatory disease of the joints. It always causes damage to bone or cartilage to some extent.
Biologically active substances are released from the destroyed cells, triggering an inflammatory response. The blood vessels in the diseased area expand and fill with blood: therefore, immune cells enter the joint tissue and fight against the destructive factors.
At the same time, the liquid part of the blood leaves the vascular bed and forms edema, thereby limiting the area of inflammation. This is the body's way of protecting itself from widespread destruction by bacteria, foreign bodies and chemicals.
After the pathogen is completely or partially eliminated, the repair mechanism is started. If the damage is small, normal tissue function is restored. Deep defects are healed by scars-areas with rough connective tissue cannot perform the normal function of the organ.
Arthritis has gone through all these stages:
- Change-damage;
- Exudation-the formation of edema;
- Diffusion-cure.
Reason
The cause of the disease is very big, we will list the main reasons:
- Streptococcal infections (tonsillitis, scarlet fever) often cause complications-rheumatism;
- Invasive autoantibodies-proteins produced by the human body that fight against its own tissues; this situation develops with the error of the immune defense system. Because of this error, she believes that the joints are foreign bodies in the body-rheumatoid arthritis;
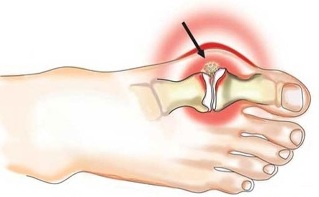
- Violation of purine metabolism can cause uric acid crystals to be deposited in the joints-gout;
- Allergic reactions can affect joint tissues and cause inflammation-allergic arthritis;
- Long-term use of certain drugs can cause inflammation (isoniazid, D-penicillin, hydralazine, small holes)-drug-induced arthritis;
- Bacteria carried in the blood or during surgery-infectious arthritis;
- Any location of viral or bacterial infections can indirectly affect joint tissue-this is reactive arthritis;
- Acute trauma-recent injury (impact, contusion, capsule rupture).
Symptoms
The disease is characterized by the acute early stage, that is, severe pain in the joints of a person under a background of complete health. For the autoimmune form, it is characterized by symmetrical injuries of the small joints-finger, wrist, elbow between the fingers.
In most cases, gout starts with inflammation of the joints between the thumb and foot. In bacterial and reactive arthritis, the large joints are usually affected on one side: knees, hips, and bones (at the junction of the spine and pelvis).
Rheumatism develops on the background of fever and general weakness, usually before angina. Fever, severe poisoning can cause severe inflammation of bones, cartilage and synovium: headache, weakness, loss of appetite.
The skin above the joints turns red and feels hotter than other areas. From the outside, it looks swollen and increases in volume. If the lesion only occurs on one side, the difference between the healthy limb and the diseased limb can be seen.
Movement limitation is related to swelling and pain. If the joint cavity is slightly inflamed, it can almost fully function. When an obvious pathological reaction occurs, the entire synovial cavity can be filled with fluid-in this case, mobility is greatly restricted.
Treatment
If the cause is mechanical damage, treatment by a general practitioner, rheumatologist or surgeon. The therapy aims to eliminate irritants and prevent inflammation.
For bacterial and reactive arthritis, antibiotics are needed, for autoimmune-cytostatics or glucocorticoids, for allergic drugs-glucocorticoids and antihistamines.
During arthroscopy, use a syringe or a special suction device to remove inflammatory fluid. During the entire process of acute inflammation, the joints are fixed. Show patients that after therapeutic exercises, joint mobility can be restored.
Doctor’s advice
Starting from the personal practice and work experience of colleagues-Inflammation of joints of any cause, gelatin application shows good symptoms. They are easy to implement and inexpensive. It is necessary to fold the gauze into several layers, and its length and width should be enough to make the joint sore. Dip the folded gauze into hot water, squeeze and straighten it. Sprinkle a thin layer of gelatin on the top and roll it up so that it fits inside like a bag without spilling. Lie on the joint, wrap it in a polyethylene bag on top, and fix it with bandages and/or tape. You can wear the compress for up to 3 hours, 2 times a day for 2 weeks. The effect can usually be felt within the first 4-5 days of use, but the treatment must be continued to achieve the desired effect. If the treatment is interrupted, the pain will recur.
What is arthropathy
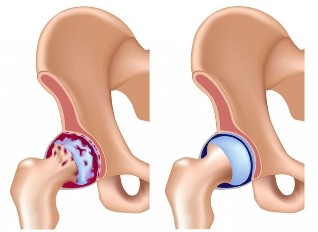
Arthritis (otherwise called osteoarthritis) is a degenerative malnutrition disease. It is based on the deterioration of articular cartilage nutrition, its recovery slows down and gradually becomes thinner.
In short, the cartilage layer wears out faster than it rebuilds. The surface of the bone and joint is exposed. They are not as smooth as cartilage and rub against each other as they move. The bone plate was partially destroyed and mild chronic inflammation appeared.
As the disease progresses, bone spurs grow in the joints-a protective tissue response to permanent damage. They can interfere with the sliding of the surfaces relative to each other and can impair joint mobility.
Osteoarthritis in most people begins to develop after 30-40 years and lasts for several years, with mild or moderate symptoms.
Vertebral osteoarthritis is often called osteochondrosis.
Reason
There are some triggers that can lead to the early development of pathology and complicate the course of the disease:
- Athletes take a lot of physical exercise;
- Obesity;
- History of joint injury;
- Vascular diseases;
- Sedentary lifestyle;
- Violation of the normal structure of joints, such as using flat feet;
- Exposure to vibration for a long time; Women
- -Hormonal imbalance or menopause.
Symptoms
usually affects the large joints on one side: knees, hips, hip bones. The disease started imperceptibly. First, pain is rarely disturbed and is related to a lot of physical activity.
If the person is able to rest, the unpleasant feeling will disappear in the same day or a few days later. As the disease progresses, the intensity of pain increases, even under normal daily pressures.
The mobility of the joints gradually decreases and is completely lost as a result of the disease. Movement of the affected limb can cause severe pain. Arthritis exacerbates osteoarthritis-fluid accumulates in the joint cavity and the skin above it becomes red and hot. After the inflammatory response subsides, the course of the disease will return to the previous course.
Treatment
Arthropathy is treated by surgeons, plastic surgeons (and sometimes surgeons). The purpose of treatment is to restore the metabolic process in the cartilage, improve the nutrition of the joints and eliminate inflammation. The treatment is lifelong and can be administered continuously or in a course of treatment.
During the attack period, a cartilage protective agent is prescribed in the form of tablets and ointments, therapeutic exercises, and massage. As the condition worsens, chondroprotectants are administered intravenously or intramuscularly together with analgesics and anti-inflammatory drugs. Traumatologists may inject protective drugs directly into the joints every few months.
The advanced stage of the disease requires surgical intervention. During this period, the diseased joint is replaced with an artificial joint.
Differences between diseases
| Features | Arthritis | Arthritis |
| Cause | Inflammation | Cartilage degeneration |
| Stream | Acute, chronic exacerbation | Chronic |
| Pain | It was strong from the beginning, and it was more obvious in the morning | Weakness at the beginning of the disease and gradually increases. Will worsen at night and after fatigue |
| Movement | It is necessary to "disperse"-in the morning after sleeping, joint mobility is the worst | The liquidity is gradually decreasing, there is no morning stiffness |
| Affected joint | The small joints of the hands and feet are affected symmetrically. Large bacterial infection | One or more large joints on different sides of the body |
| blood test | General blood test, severe inflammatory changes of rheumatoid factor, C-reactive protein, pathogen antibody | No typical changes |
| X-ray | Stage changes, osteoporosis-bone loss, cysts in the bones | Gradually change, the joint space is deformed, the appearance of bone spurs and bone growth. |
| Basic treatment | Anti-inflammatory drugs | Cartilage protector |
The similar characteristics of the two diseases are the progressive course and the gradual loss of mobility. When a person is still frivolous about his health, autoimmune arthritis usually appears at a young age.
It must be remembered that any joint pain that persists for a long time can occur under certain circumstances-this is a serious reason to see a doctor. It is important to diagnose the disease in time and start treatment to slow down the development of the pathological process.



































